If the butterfly effect refers to the wide-ranging effects of a small act, what do you call the fallout from a cataclysmic event? A bevy of studies are now revealing the many repercussions of the COVID-19 pandemic.
The hopes that increased use of personal protective equipment, patient isolation, and a heightened sense of emergency might have led to a decrease in healthcare-associated infections (HAIs) during the pandemic have been dashed by two major studies recently published.
Both studies, one published in Clinical Infectious Diseases and the other in Infection Control & Hospital Epidemiology, draw from the US National Healthcare Safety Network’s (NHSN) database of reported HAI events, though the one published by Oxford University Press conducted an additional survey of 148 hospitals during 2020. While they do not fully share each others’ datasets, these studies draw similar conclusions.
US healthcare system: Things were getting better
Particularly heartbreaking for infection control practitioners, COVID-19 quickly undid years of improvement. In America, there had been “consistent, significant reductions” in infection rates across a range of infections from 2015 to 2019.[1] This trend continued in the first quarter of 2020.[2] Progress was still being made prior to the arrival of COVID-19 in the United States.
“We lost nearly a decade of progress”
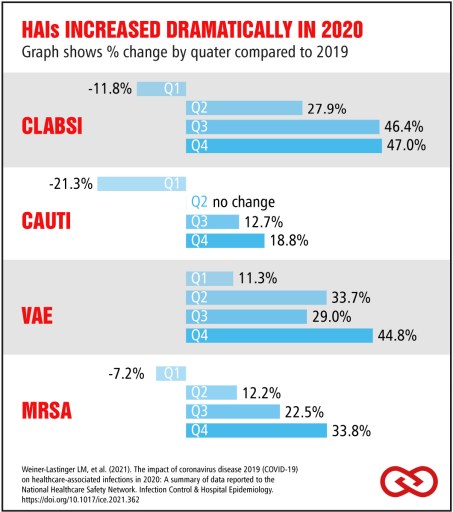
In response to this new data, APIC President Ann Marie Pettis lamented these pandemic-related changes. “The unfortunate reality is that in one year we lost nearly a decade of progress against HAIs like central line-associated bloodstream infections [CLABSI], catheter-associated urinary tract infections [CAUTI], methicillin-resistant Staphylococcus aureus (MRSA), and ventilator-associated events [VAE].” [3]
The dramatic increase in these infections can be seen quarter-to-quarter.
Increased HAIs, decreased reporting
The increase of COVID-19 infections also corresponded to weakened reporting. While the number of hospitals reporting data to the NHSN per quarter remained broadly consistent throughout 2019, there was a drop in the number of hospital reporting infection rates in 2020. This was especially pronounced in the decrease in hospitals reporting data for VAE and SSI infections, a drop of 22-36%. [4]
Baker, et al conclude that “facilities may have been challenged [by the increased workload], leading to reduced reporting.” [5]
Corresponding spikes in COVID-19 infections and HAIs
The studies theorize that the rise of COVID-19 cases did not just reduce the reporting capacity of hospitals. Instead, “negative impacts may have resulted when usual efforts to monitor and prevent HAIs were redirected to the COVID-19 response.”

Baker et al looked at the relationship between HAI clusters and COVID-19 discharges per month, and the corresponding effect can be seen in the graphic.
Systems—and people—suffered
The increase in HAIs and decrease in hospitals able to report reveal a healthcare system already stretched thin, primed for efficiency instead of resiliency. This is also shown in the cost the pandemic had on healthcare worker’s mental health.[6]
Our Medical Director, Dr. Glockner, addressed this issue earlier in the pandemic. “As we consider the future of infection prevention, one of the most important needs is to increase the number of healthcare workers per patient to decrease the workload. (This is true in the most countries of the world, including Germany.)”
Ann Marie Pettis also emphasized the need for relief, speaking of the need to “support [healthcare workers] with adequate resources so that they can handle emerging threats to public health.”[7]
One bright spot
Of all the infections that were tracked, there was one that did not increase during the pandemic, C. difficile (CDI). The rates of CDI remained stable or decreased during 2020. The theory is that the increase in “barrier precautions and increased training on donning and doffing of PPE to prevent COVID-19 transmission might have led to reductions in the carriage of C. difficile.” [8]
CDI rates are an outlier but may give us hope for how to improve infection prevention as the pandemic slows and ends.
These studies concluded that the capacity for preventing HAIs needs to be increase. “Our results identify a need to build capacity in infection prevention and control. As hospitals prepare for the next stages of the pandemic and recovery, this study emphasizes the need to remain focused on routine infection prevention.” [9]
Sources:
[1] Wu, Hsiu, et al. “Hospital Capacities and Shortages of Healthcare Resources among US Hospitals during the Coronavirus Disease 2019 (COVID-19) Pandemic, National Healthcare Safety Network (NHSN), March 27–July 14, 2020.” Infection Control & Hospital Epidemiology, 24 June 2021, p. 1.
[2] Wu, Hsiu, et al. p. 12.
[3] HAI Increases.” APIC, apic.org/news/statement-from-apic-president-ann-marie-pettis-bsn-rn-cic-fapic-about-hai-increases/.
[4] Wu, Hsiu, et al. p. 2.
[5] Baker, Meghan A, et al. “The Impact of COVID-19 on Healthcare-Associated Infections.” Clinical Infectious Diseases, 9 Aug. 2021, 10.1093/cid/ciab688.
[6] Kachadourian, Lorig K., et al. “Transdiagnostic Psychiatric Symptoms, Burnout, and Functioning in Frontline Health Care Workers Responding to the COVID-19 Pandemic.” The Journal of Clinical Psychiatry, vol. 82, no. 3, 27 Apr. 2021, 10.4088/jcp.20m13766. Accessed 28 May 2021.
[7] “Statement from APIC President, Ann Marie Pettis, BSN, RN, CIC, FAPIC, about HAI Increases.” APIC, apic.org/news/statement-from-apic-president-ann-marie-pettis-bsn-rn-cic-fapic-about-hai-increases/.
[8] Baker, Meghan A, et al. p. 6.
[9] Baker, Meghan A, et al. p. 6.














Kommentieren